Assessing Biogen’s Strategic Move into Oral Macrocyclic Peptides: A Clinical Viability Report
The pharmaceutical landscape for immunological conditions may be on the verge of a major shift. Biogen Inc.’s new collaboration with Dayra Therapeutics marks a strategic move into the growing field of oral macrocyclic peptides.
Biogen is investing $50 million upfront, with more milestone payments possible as the program advances. The deal structure shows strong confidence in this emerging drug class and its potential impact on chronic inflammatory and autoimmune diseases.
For patients, the implications could be significant. Oral macrocyclic peptides may improve treatment adherence and therapeutic outcomes, and could eventually challenge the current dominance of injectable biologics in immunology.
The Core Analysis: A New Modality for Immunological Targets
Biogen has a market capitalization of more than $25 billion. Its stock has surged nearly 40% over the past six months. The company is now making a clear move to diversify its early-stage portfolio.
The new collaboration with Dayra Therapeutics focuses on discovering and developing oral macrocyclic peptides. These candidates will target a range of immunological conditions.
This isn’t just another incremental drug development; it’s a strategic embrace of a modality that seeks to combine the best attributes of small molecules and biologics.
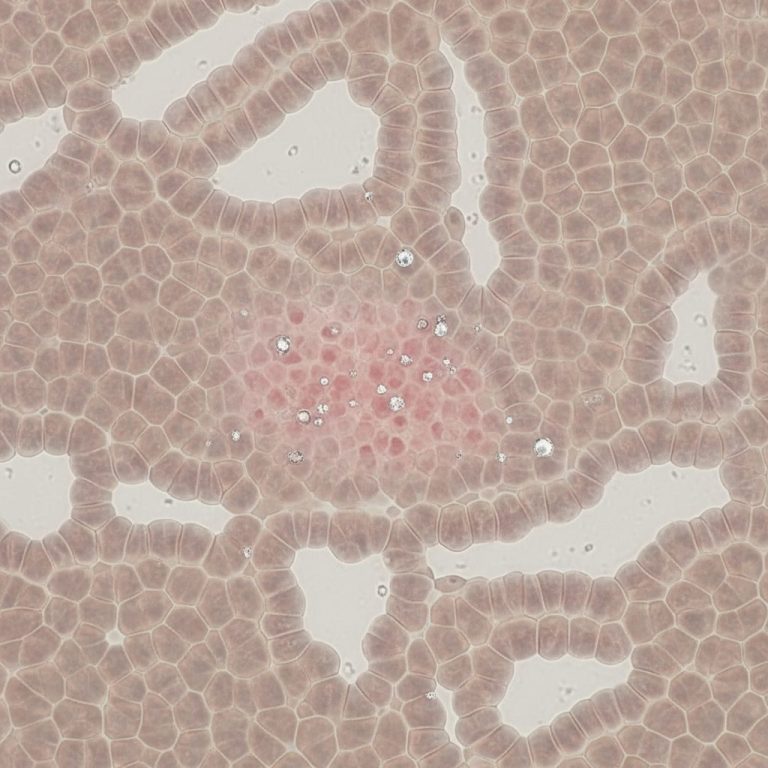
Oral macrocyclic peptides are molecules with a cyclic structure. This design improves stability and can enhance cell permeability compared to linear peptides.
Clinically, what makes them exciting is their potential to match the specificity of large biologics. Yet, they may deliver that level of precision in an oral format. For patients, that convenience is close to a “holy grail.”
Traditional small molecules, while orally bioavailable, often lack the precise targeting capability of biologics, leading to off-target effects. Conversely, biologics, despite their exquisite specificity, are typically large proteins requiring parenteral administration, which can be burdensome for patients managing chronic conditions¹.
This is where oral macrocyclic peptides truly shine, bridging a critical gap in drug delivery and mechanism of action (MOA).
Dayra Therapeutics, founded in 2024 by Versant Ventures, brings a specialized platform to the field. It combines macrocycle discovery with advanced computational design.
This approach helps identify and optimize complex molecules more efficiently. It also enables targeting disease-relevant proteins that are often inaccessible to conventional small molecules.
Many critical protein-protein interactions (PPIs) are central to immunological signaling pathways. These targets have large, flat, and dynamic binding sites that rigid small molecules struggle to inhibit.
Biologics, with their larger surface areas, can engage these targets, but again, the delivery limitation persists.
Oral macrocyclic peptides, due to their size and conformational flexibility, are uniquely positioned to modulate these challenging PPIs, offering a novel therapeutic approach where existing modalities fall short².
The current partnership is firmly in the discovery and preclinical development stage. This means Dayra will lead the initial identification, validation, and optimization of these candidates. Following this, Biogen will take the reins for further development, potential commercialization, and manufacturing. While no specific efficacy or safety data are available yet given the nascent stage of the collaboration the promise lies in their inherent design.
The ability to target intracellular proteins or complex extracellular protein interfaces with high specificity, combined with oral delivery, could reshape the treatment landscape for conditions like inflammatory bowel disease, rheumatoid arthritis, and lupus.
For patients, shifting from frequent injections or infusions to a once-daily pill may greatly improve comfort, adherence, and overall quality of life key priorities in long-term disease management.
The financial terms reinforce Biogen’s commitment. The $50 million upfront payment, recorded as an Acquired In-Process R&D expense in Q4 2025, signals confidence in early innovation. Future milestone payments create incentives for Dayra to advance candidates through preclinical research and early clinical development, aligning both companies toward successful progress.
Regulatory and Timeline Assessment of Oral Macrocyclic Peptides
The development pathway for a new drug class like oral macrocyclic peptides comes with both opportunities and challenges. Even when the immunological targets are well understood, translating a novel modality into a safe and effective therapy is complex.
Right now, the Biogen–Dayra program is still in the discovery and preclinical phase. This early stage is crucial, and it’s also where most drug candidates fail. Success depends on strong data, careful optimization, and a clear safety profile before clinical trials can begin.
For an oral macrocyclic peptide candidate to progress, it must first demonstrate robust proof-of-concept in in vitro and in vivo preclinical models, confirming both target engagement and therapeutic effect in relevant disease models.
Simultaneously, rigorous pharmacokinetic (PK), pharmacodynamic (PD), and toxicology studies are paramount to establish a favorable safety profile and predictable drug metabolism. The “oral” aspect, while a clinical advantage, adds another layer of complexity to these studies.
Ensuring adequate oral bioavailability, stability in the gastrointestinal tract, and acceptable drug-drug interaction profiles are formidable hurdles that many peptide-based drugs struggle to overcome.
Assuming successful preclinical data, the next major regulatory milestone would be the submission of an Investigational New Drug (IND) application to regulatory bodies like the FDA in the United States or the EMA in Europe. An IND allows for initiation of human clinical trials.
Given that Dayra was founded in 2024 and the collaboration announced in late 2025, a realistic timeline for an IND filing would likely be in the late 2020s to early 2030s. This early timeline accounts for the extensive optimization, lead selection, and preclinical studies required.
Upon IND acceptance, the molecule would enter Phase 1 clinical trials, focusing primarily on safety, tolerability, and initial PK/PD in healthy volunteers. If successful, Phase 2 trials would then commence in patient populations, aiming to establish preliminary efficacy and optimal dosing.
For immunological conditions, these trials often involve specific biomarker measurements and clinical outcome assessments relevant to the disease. A positive outcome here would then lead to Phase 3 trials, which are large-scale, pivotal studies designed to confirm efficacy, monitor adverse events, and gather data for regulatory approval.
The regulatory environment for novel modalities is generally supportive, especially if the new drug addresses significant unmet needs or offers substantial advantages over existing therapies. The oral route for biologics-like specificity in chronic immunological conditions unequivocally ticks both boxes. However, regulators will scrutinize the safety profile of these novel molecules meticulously.
The cyclic structure, while beneficial for stability, can sometimes introduce unexpected toxicities or off-target interactions that must be thoroughly de-risked.
Projected Timeline for First Oral Macrocyclic Peptide Candidate (from this collaboration):
- 2025-2029: Discovery & Preclinical Development
- Late 2029 – Early 2031: IND Filing & Phase 1 Clinical Trials
- 2031-2034: Phase 2 Clinical Trials
- 2034-2037: Phase 3 Clinical Trials & Regulatory Submission
- 2037-2038+: Potential Market Approval
This timeline is, of course, optimistic and contingent on a smooth development path, which is rarely the case in pharmaceutical R&D. Nonetheless, Biogen’s decision to invest early suggests a long-term strategic vision.
Clinical Snapshot: Biogen/Dayra Oral Macrocyclic Peptides
Target Indication: Immunological Conditions (e.g., autoimmune diseases, chronic inflammation)
Current Phase: Discovery/Preclinical (Early Research Collaboration)
Mechanism of Action: Oral macrocyclic peptides targeting protein-protein interactions (PPIs) and other challenging protein binding sites.
Key Potential Results/Benefits:
- Oral administration, significantly improving patient convenience and adherence compared to injectable biologics.
- Biologics-like specificity and potency due to their larger size and conformational flexibility, enabling modulation of complex biological pathways.
- Ability to target intracellular pathways and previously “undruggable” protein interfaces that are inaccessible to traditional small molecules and challenging for biologics.
- Potential for reduced immunogenicity compared to large protein biologics.
Current Safety/Efficacy Data: Not yet applicable; currently in preclinical research. Focus is on establishing robust preclinical proof-of-concept and safety.
Expanding the Context: Why This Matters Now
Biogen’s move isn’t happening in a vacuum. The broader peptide therapeutics market is experiencing significant growth, driven by advancements in peptide synthesis, computational design, and an increasing understanding of peptide pharmacology.
The global peptide therapeutics market, valued at approximately $45-50 billion in 2023, is projected to reach over $80 billion by the early 2030s, fueled largely by innovation in oncology, metabolic disorders, and immunology³. Within this, oral peptides represent a frontier with immense commercial potential, provided the bioavailability and stability challenges can be consistently overcome.
Other major pharmaceutical companies are also exploring macrocyclic peptide programs, though not all are focused on oral delivery in immunology. Interest in this space is growing because these molecules offer a rare combination: biologic-level specificity with the potential for oral bioavailability. This makes macrocyclic peptides an increasingly attractive investment area.
Dayra Therapeutics’ explicit focus on leveraging computational design to overcome traditional macrocycle development hurdles is a critical differentiator. This computational approach allows for faster screening of vast chemical spaces and more efficient optimization of lead candidates, potentially accelerating the often-arduous drug discovery process⁴.
Furthermore, Biogen has demonstrated a proactive approach to pipeline diversification and innovation recently. The company’s recent regulatory success with high-dose nusinersen for 5q spinal muscular atrophy and the acquisition of Alcyone Therapeutics’ ThecaFlex DRx drug delivery system underscore a commitment to both innovative therapies and novel delivery mechanisms.
This partnership with Dayra aligns perfectly with this broader strategy, indicating a willingness to invest in disruptive technologies that could yield next-generation therapeutics.
Short- and Long-Term Outlook of Oral Macrocyclic Peptides
The short-term outlook for the Biogen-Dayra collaboration is one of intense preclinical research and optimization. Success in this phase hinges on Dayra’s platform delivering novel macrocyclic peptide candidates that demonstrate not only potent target engagement but also favorable pharmacokinetics and a clean safety profile in in vivo models.
Biogen’s financial commitment ensures Dayra has the resources to pursue these challenging early-stage goals. We can anticipate regular updates on preclinical progress over the next 2-3 years, with the critical inflection point being an Investigational New Drug (IND) filing.
The long-term outlook, while inherently speculative given the early stage of development, is exceptionally promising. If Biogen and Dayra can successfully bring an orally bioavailable macrocyclic peptide targeting a high-value immunological condition to market, it could represent a significant competitive advantage.
The ability to offer a convenient oral alternative to injectable biologics would greatly enhance patient compliance, potentially improve clinical outcomes, and capture a substantial market share in an already massive and growing therapeutic area.
This venture positions Biogen at the forefront of a potentially transformative drug class, offering a compelling blend of clinical innovation and commercial opportunity for the years to come.
Stay ahead of the clinical curve—the next great peptide is already in Phase 2. 💊
References
- Investopedia. (2025, November 24). Biogen Partners with Dayra to Develop Oral Macrocyclic Peptides.
- Versant Ventures. (n.d.). Dayra Therapeutics: Precision Oral Macrocycles. (Accessed for company background and scientific focus)
- Grand View Research. (2023). Peptide Therapeutics Market Size, Share & Trends Analysis Report By Type (Innovator, Generic), By Application (Cancer, Metabolic, CVD), By Route of Administration (Parenteral, Oral), By Synthesis Technology, By Region, And Segment Forecasts, 2023 – 2030. (Accessed for market projections and trends)
- Nature Reviews Drug Discovery. (2022). Macrocyclic peptides: a new frontier in drug discovery. (Accessed for general information on macrocyclic peptides and their potential in drug discovery, particularly computational design aspects).
All human research MUST be overseen by a medical professional