Revolutionizing Antimicrobial Peptide Discovery: Assessing the Clinical Viability Impact of CG-AMP
Antibiotic resistance continues to grow at a pace that outmatches current drug development methods. Researchers estimate that resistant infections may cause up to 10 million deaths per year by 2050 if new therapeutics do not emerge. The race is not just urgent. It is personal for every clinician, researcher, and policymaker working to prevent a post-antibiotic era. One promising direction is CG-AMP antimicrobial peptide discovery.
Antimicrobial peptides, or AMPs, have become a strong candidate class because they show broad activity against bacteria, fungi, and viruses. They often damage pathogens through membrane disruption, which reduces the likelihood of resistance compared to traditional antibiotics.
However, identifying and optimizing AMPs takes time, funding, and extensive laboratory screening. That is why advanced computational frameworks such as CG-AMP are beginning to reshape the landscape. These tools accelerate discovery and help researchers evaluate which peptides are most likely to succeed in preclinical and clinical testing.
Why CG-AMP Antimicrobial Peptide Discovery Matters Right Now
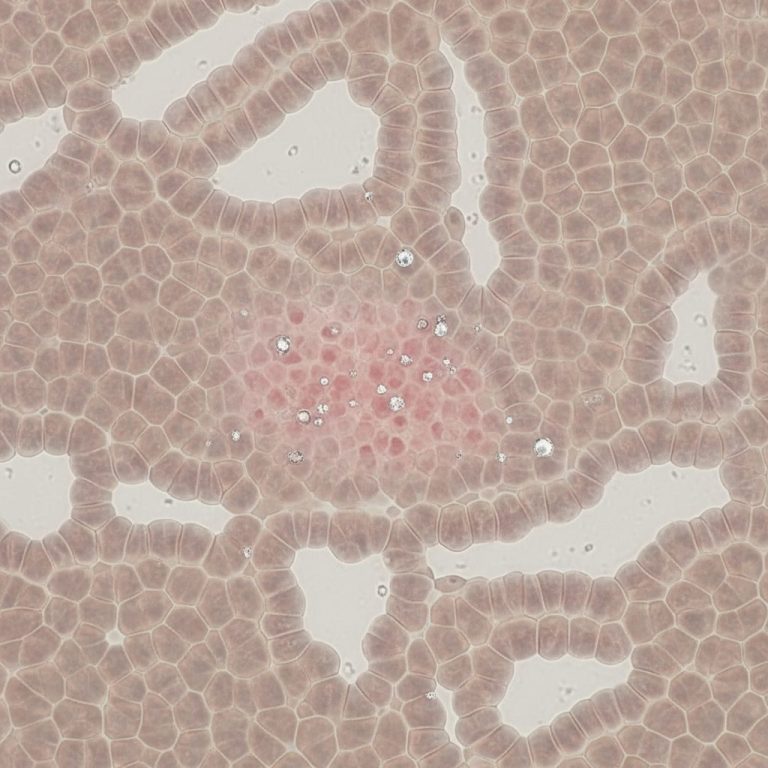
Traditional AMP discovery methods rely on wet lab screening. This process is slow, expensive, and inefficient when facing fast-evolving pathogens. AMPs vary in structure, length, charge, and stability. Without predictive tools, researchers sort through thousands of sequences before finding promising candidates.
CG-AMP antimicrobial peptide discovery helps solve this bottleneck. Instead of screening every peptide manually, CG-AMP predicts which candidates have the highest chance of antimicrobial activity and safety. This approach brings machine learning into early drug discovery and gives researchers a head start before laboratory validation begins.
Transitioning from random search to intelligent prioritization is not just innovative. It is necessary to keep pace with superbugs and reduce early-stage drug failure.
How CG-AMP Works
CG-AMP is a deep learning framework built to analyze peptide sequences at scale. The model has two key modules. Each supports antimicrobial prediction from a different perspective.
Module 1: Language Model and Contrastive Learning
Protein and peptide sequences behave like structured language. Each amino acid represents a token and each pattern contributes meaning. CG-AMP uses a pre-trained language model to understand this structure. It learns the biological grammar behind effective antimicrobial peptides.
Contrastive learning improves this process by teaching the model to distinguish between real AMPs and non-effective peptides. This helps the system focus on meaningful patterns rather than memorizing training examples.
Module 2: Enhanced Convolutional Neural Network
The second module uses an enhanced convolutional neural network to find detailed sequence patterns. CNNs are known for recognizing spatial signals in images. In this context, CNNs detect biochemical motifs, charge patterns, and structural elements essential for AMP function.
By combining both modules, CG-AMP creates a strong feature representation. The system analyzes peptides from multiple angles and produces prediction outputs that are more accurate than earlier models.
Measured Performance of CG-AMP
CG-AMP was evaluated using two benchmark test sets. The results demonstrate high accuracy and consistency:
| Dataset | Accuracy | F1 Score | MCC |
|---|---|---|---|
| AMPlify Test Set | 0.9497 | 0.9508 | 0.8994 |
| DAMP Test Set | 0.9403 | 0.9392 | 0.8812 |
A high Matthew’s Correlation Coefficient signals balanced predictions for both positive and negative samples. This reduces costly experimental false positives.
These results place CG-AMP among the strongest computational screening tools available for AMP identification.
Clinical Relevance of CG-AMP Antimicrobial Peptide Discovery
CG-AMP itself is not a therapeutic agent. Instead, it supports the drug discovery process by improving the efficiency of selection and optimization. Early drug development is the most expensive and uncertain phase. Many candidates fail because they lack potency, stability, or safety.
Using CG-AMP antimicrobial peptide discovery can:
- Reduce the number of unnecessary experiments
- Prioritize high-potential peptide families
- Support mechanistic research
- Help identify peptides active against resistant pathogens
- Shorten the time between concept and preclinical trials
This efficiency is valuable because regulators such as the FDA and EMA increasingly support computational models within submissions. Predictive modeling can strengthen the scientific rationale for proceeding to in vivo testing and reduce uncertainty during Investigational New Drug filings.
Regulatory Landscape and Timeline Considerations
Computational workflows are gaining acceptance in regulated industries. Agencies encourage model-informed development when supported by evidence. Although CG-AMP does not replace biological testing, it can complement it by improving candidate quality early in the timeline.
For example, if CG-AMP predicts that a peptide has properties suitable for targeting multidrug-resistant bacteria, those data can support applications for:
- Fast track designation
- Orphan drug status
- Priority review
These pathways may significantly shorten development timelines for life-saving antimicrobial products.
The Road Ahead for AMPs and CG-AMP
The pipeline of traditional antibiotics is shrinking. At the same time, global demand for new antimicrobial categories is rising. AMPs offer potential benefits including immune modulation, synergy with existing antibiotics, and reduced resistance.
CG-AMP antimicrobial peptide discovery may help identify new peptide families suitable for clinical translation. As more datasets become available, deep learning models will continue to improve. With time, these tools may predict toxicity, stability, and pharmacokinetics, not just antimicrobial activity.
In the short term, CG-AMP will likely introduce more validated AMP candidates into early research pipelines. In the long term, it may accelerate the next generation of antimicrobial drugs that reach clinical trials and patient use.
Final Thoughts
The future of antibiotic development depends on speed, accuracy, and innovation. CG-AMP antimicrobial peptide discovery is part of a growing transition from traditional biology to computationally assisted research. It reduces discovery uncertainty and enables smarter prioritization in an area where every month counts.
The next breakthrough antimicrobial may not be found in a petri dish. It may begin as a predicted sequence in a machine learning model and reach patients faster because of it.
The science is accelerating. The world is watching. And CG-AMP is helping lead the way.
Stay ahead of the clinical curve—the next great peptide is already in Phase 2. 💊
References
- O’Neill, J. (2016). Tackling drug-resistant infections globally: final report and recommendations. The Review on Antimicrobial Resistance.
- U.S. Food and Drug Administration. (2023). Advancing Regulatory Science for Drug Development. Retrieved from https://www.fda.gov/drugs/regulatory-science-research-and-development/advancing-regulatory-science-drug-development
- European Medicines Agency. (2022). Guideline on the clinical development of medicinal products for the treatment of bacterial infections. Retrieved from https://www.ema.europa.eu/en/documents/scientific-guideline/guideline-clinical-development-medicinal-products-treatment-bacterial-infections-revision-1_en.pdf
All human research MUST be overseen by a medical professional